In February 2022 CMPT sent a simulated tissue biopsy proficiency testing challenge with a history of a 79 year old quadriplegic, long-term care resident, with bed sore ulcer.
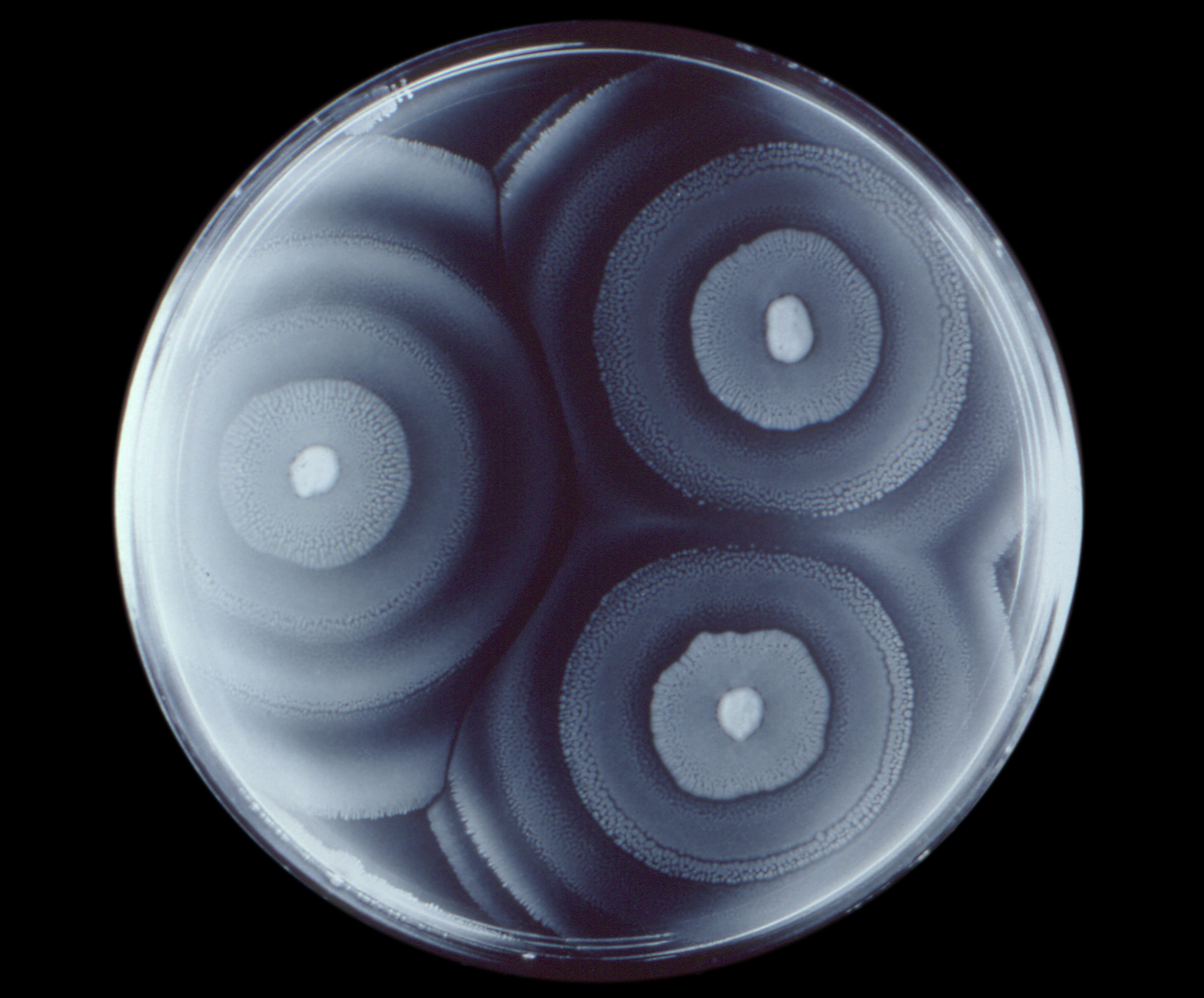
The sample contained a Proteus mirabilis that was susceptible to ampicillin and resistant to cefazolin.
66% or the participants reported the strain susceptible to ampicillin and resistant to cefazolin, however, 34% of the labs reported ampicillin as resistant despite obtaining low MIC values.
CMPT graded the reporting of ampicillin as resistant in this case, unacceptable. Two laboratories challenged the grade indicating their protocols would change the result of ampicillin to resistant if cefazolin tested resistant.
The Clinical Bacteriology Technical Committee reviewed the appeals and decided the grade would stand.
Below is the response to the appealing laboratories.
Thank you for your recent correspondence regarding challenge M214-2. Fundamentally, the issue lies in whether there is a resistance mechanism present to cefazolin in this organism at all.
The epidemiologic distribution of cefazolin MICs in wild-type P. mirabilis populations are significantly higher than for E. coli, on which the newest breakpoints were primarily based. In CLSI’s rationale for the testing breakpoint change to the current values in 2010, they point out, “Even wild-type P. mirabilis is less susceptible to cefazolin and first-generation cephalosporins in general. The modal MIC of wild-type P. mirabilis is 4 mg/L, compared with 1 mg/L for E. coli and 2 mg/L for Klebsiella species.” (1)
This is further borne out by the epidemiological data publicly available at http://mic.eucast.org. The wild-type populations of P. mirabilis have higher MICs against cefazolin than E. coli, in the absence of any resistance mechanism. This same MIC elevation is not seen with ampicillin against P. mirabilis. The calculated epidemiologic cut-off value for P. mirabilis against cefazolin is 8 mg/L, which would be considered resistant given the CLSI current breakpoints.
Furthermore, the data in CLSI’s rationale for the testing breakpoint change indicates that >96% of ampicillin-susceptible P. mirabilis isolates test non-susceptible (I or R) to cefazolin. (1) Given this, reflexively flipping the ampicillin interpretation to match the cefazolin interpretation would generate a tremendous number of major errors and inappropriately limit the use of ampicillin in highly susceptible, wild-type isolates, which would be injurious to antimicrobial stewardship.
Given the above, the committee maintains its position, consistent with CLSI guidelines, that ampicillin should be reported independently of cefazolin, particularly in the context of P. mirabilis, and should be based on the interpretive breakpoints outlined by CLSI in their most recent guidance document. As such, we regret to inform you that the committee will not be changing the grading for this challenge.
Sincerely,
Clinical Bacteriology Technical Committee



