So you would love to feel like this?
But instead you look like this?
You are not alone …
Onychomycosis affects over 35 million people in the United States alone;(1) the disease has a prevalence of approximately 3% of the adult population in North America and Europe.(2)
Dermatophytes are the most frequently implicated causative agents in onychomycosis (nearly 90% in toe nail and at least 50% in fingernail infections); the most common being Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum although variation exists worldwide.(3),(4)
A healthy nail is not usually susceptible to fungal infection; predisposing factors include age, circulatory disorders affecting the lower extremities, metabolic disorders such as diabetes mellitus, and immunosuppressive conditions.(2),(5)
Diagnosis
 Laboratory confirmation of onychomycosis should be obtained before starting treatment and both for direct microscopy and in vitro laboratory culture should be performed.(3)
Laboratory confirmation of onychomycosis should be obtained before starting treatment and both for direct microscopy and in vitro laboratory culture should be performed.(3)
Direct microscopy is the first screening tool used to identify fungal structures as identification of dermatophytes requires approximately 2–6 weeks.
KOH and Calcofluor white are the two most common techniques for direct examination. Calcofluor white binds to cellulose and chitin and fluoresces when exposed to ultraviolet radiation increasing sensitivity but the need of a fluorescent microscope limits its use.(4)
Treatment
Although many people think than onychomycosis is only a cosmetic problem, the infection can cause problems beyond the esthetic appearance.
Infected nails may serve as a reservoir of fungi with a potential for spread to the feet, hands and groin.(2) Further complications can occur also in diabetic and immunocompromised patients.(1)
Is there hope?
Current approaches to treatment include systemic therapy, mechanical/surgical, topical therapy, or a combination of these.(1)
Systemic therapy
The main systemic drugs approved and used for the treatment of onychomycosis are terbinafine, itraconazole, and griseofulvin.2 Terbinafine is considered the gold standard with cure rates of >70%.6
Medical debridement
Debridement reduces the thickness of the nail and decreases the fungal load but does not address the fungus itself.(1)
Topical treatment
Topical treatments have a low success rate as the structure of the nail acts as a barrier for drug diffusion.(2) Cure and success rates have been between 8.5% and 18% after 48 weeks treatment.(7)
When evaluating treatment success it is important to understand the definitions of treatment success.
Mycologic cure means negative KOH examination and culture while Complete cure means 0% clinical involvement of the target toenail in addition to a negative KOH examination and fungal culture.(1)
Unfortunately, 100% success on these definitions is rarely achieved.
The fungi
Members of the genus Trichophyton possess several virulence factors including acid proteinases, elastase, keratinases and other proteinases that allow them to invade the keratinous tissues of humans and animals. (8)
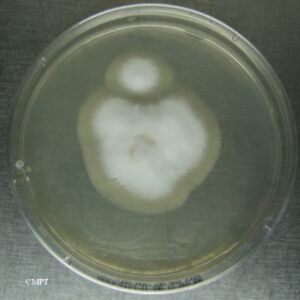
Trichophyton rubrum
T. rubrum is an anthropophilic dermatophyte, as it almost exclusively infects humans. Infections are more common in adults and men than in children and women. (9)
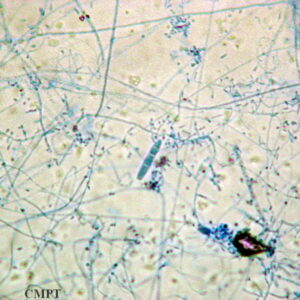
T. rubrum colony on Saboureaud agar (left), and microscopic characteristics (right): Lacto-phenol cotton blue stain under magnification of 400X

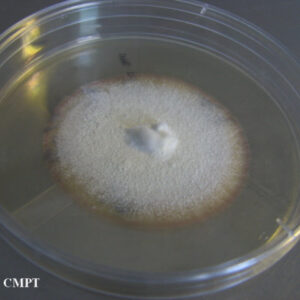
Trichophyton mentagrophytes
T. mentagrophytes is an anthropophilic fungus distributed worldwide and a common cause of tinea pedis, and sometimes superficial nail plate invasion. (10)
T. mentagrophytes colony on Saboureaud agar (left), and microscopic characteristics (right): Lacto-phenol cotton blue stain under magnification of 400X
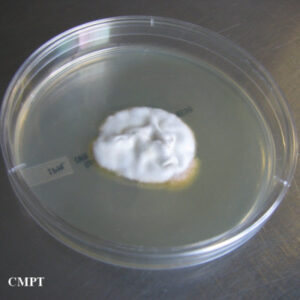
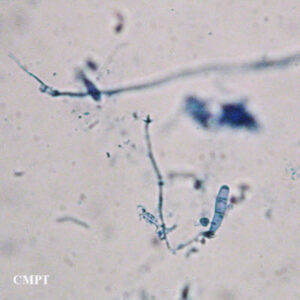
Epidermophyton floccosum
Humans are the primary host of Epidermophyton floccosum, the only species of the genus known to be pathogenic. (10) E. floccosum infections usually occur on the skin of the torso, limbs, soles of feet or palms of hands and nails. (11)
E. floccosum colony on Saboureaud agar (left), and microscopic characteristics (right): Lacto-phenol cotton blue stain under magnification of 400X
References
1. Warren J, Pollak R, Vlahovic T, Caldwell B, Jennings M, Ashton S, Markinson B, Reyzelman A, Lifshen J, Goldsmith H. Onychomycosis and the Role of Topical Antifungals Suppl Podiatry Today Nov 2013
2. Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists’ guidelines for the management of onychomycosis 2014. Br J Dermatol. 2014;171:937-958.
3. Elewski BE. Onychomycosis: Pathogenesis, Diagnosis, and Management. Clin Microbiol Rev. 1998;11:415-429.
4. Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol. 2010;28:151-159.
5. Nenoff P, Kruger C, Ginter-Hanselmayer G, Tietz HJ. Mycology – an update. Part 1: Dermatomycoses: causative agents, epidemiology and pathogenesis. J Dtsch Dermatol Ges. 2014;12:188-209; quiz 210, 188-211; quiz 212.
7. Gupta AK, Fleckman P, Baran R. Ciclopirox nail lacquer topical solution 8% in the treatment of toenail onychomycosis. J Am Acad Dermatol. 2000;43:S70-80.
8. Summerbell RC. Trichophyton, microsporum, epidermophyton, and agents of superficial mycoses. In: Versalovic ea, ed. Manual of Clinical Microbiology. Vol 2. 10th ed. ed. Washington, DC.: ASM; 2011:1919.
9. Kwon-Chung K.J., Bennet J.E. Dermatophytoses (ringworm, tinea, dermatomycosis). In: Medical Mycology. Malvern, Pennsylvania: Lea & Febiger; 1992:105.
10. Larone Davise H. Medically Important Fungi. A Guide to Identification 5th Ed. 4th ed. Washington DC: ASM Press; 2011.
11. Tchernev G, Penev PK, Nenoff P, et al. Onychomycosis: modern diagnostic and treatment approaches. Wien Med Wochenschr. 2012.
6. Gupta AK, Ryder JE, Johnson AM. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol. 2004;150:537-544.




