
by Lorraine Campbell
Aminoglycoside antibiotics are derived from compounds produced by a variety of soil actinomycetes and have a similar structure consisting of two or more amino sugars linked by glycosidic bonds to an aminocyclitol ring (streptidine or 2-deoxy-streptamine).1 The commonly used agents in Canada include gentamicin, tobramycin, streptomycin, and amikacin (and topical neomycin). Other aminoglycosides in use elsewhere or of historical interest include kanamycin and netilmicin; aminogylcosides are bactericidal agents that function by inhibiting bacterial protein synthesis, they have a narrow therapeutic-to-toxic ratio, and are often used in the treatment of serious aerobic gram negative infections.2 Some have activity against mycobacteria and others are used in combination with β-lactams for synergy. Bacterial resistance to aminoglycosides can be attributed to three mechanisms: (i) decreased drug uptake, whether by decreased cell permeability or expulsion by efflux pumps, (ii) modification of the target 16S ribosomal RNA (rRNA) binding site by mutation or methylation, and (iii) enzymatic deactivation of the aminoglycoside through expression of aminoglycoside-modifying enzymes (AMEs).4
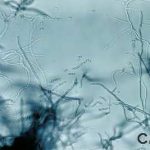
Streptomyces species. Image courtesy of Public Health Image Library
ORIGIN
Naturally occurring aminoglycosides are derived from the actinomycete Micromonospora spp. (gentamicin) or from Streptomyces spp. (kanamycin, neomycin, streptomycin and tobramycin), whereas amikacin is the semisynthetic derivative of kanamycin. The difference in spelling denotes the origin of the antibiotic: –micin indicates derivation from Micromonospora spp and –mycin from Streptomyces spp.2 Streptomycin was the first antibiotic in the aminoglycoside family to be utilized (in the 1940s), and was extrapolated from a strain of Streptomyces griseus.




